Foot pain is a widespread concern that can significantly affect daily activities and quality of life. Understanding its symptoms, underlying causes, diagnostic processes, and available treatments is crucial for effective management and prevention.
Symptoms of Foot Pain
Foot pain can manifest in various forms and locations, depending on the underlying issue. Common symptoms include:
- Aching, throbbing, or sharp pain in the heel, arch, toes, sole, or instep
- Swelling, redness, or warmth in the affected area
- Numbness or tingling, especially with nerve involvement
- Tenderness to touch, difficulty walking or bearing weight
- Stiffness, reduced range of motion, or joint deformities (e.g., bunion, hammertoe)
- Changes in skin color or texture, such as calluses, corns, or ulcers
Other symptoms may include visible deformities, bruising following trauma, and pain that intensifies with specific activities or footwear.
Common Causes of Foot Pain
Foot pain can arise from a multitude of causes, generally classified as injuries, chronic conditions, structural problems, or systemic medical disorders.
1. Injuries
- Sprains & strains: Overstretching or tearing of ligaments/tendons
- Fractures: Broken bones (toe, foot, or ankle) due to trauma or overuse
- Stress fractures: Tiny cracks in bones from repetitive impact
2. Chronic and Structural Conditions
- Plantar fasciitis: Inflammation of the tissue band across the foot bottom, causing heel and arch pain
- Bunions & hammertoes: Structural deformities of the toes or joints
- Flat feet (fallen arches): Lack of a natural arch, causing pain and fatigue
- Bone spurs: Outgrowths on bones, often at heel or toes
3. Medical & Systemic Disorders
- Arthritis: Osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and gout can cause joint pain, swelling, and deformity; big toe often affected
- Peripheral/diabetic neuropathy: Nerve damage leading to numbness, tingling, or burning
- Tarsal tunnel syndrome: Nerve compression near the ankle
4. Other Common Causes
- Morton's neuroma: Nerve thickening, often between the toes
- Calluses and corns: Thickened skin due to friction or pressure
- Warts or infections: Plantar warts (viral), fungal infections (athlete’s foot)
- Ill-fitting shoes or high heels: Leading to abnormal pressure points
Diagnostic Tests for Foot Pain
Accurate diagnosis involves a combination of clinical evaluation and targeted tests:
Clinical Assessment
- Medical history: Duration, location, nature of pain, exacerbating factors, injury history, footwear habits, and any relevant family or medical background.
- Physical examination: Includes inspection for deformities, palpation to identify tenderness, assessment of range of motion, gait analysis, neurological and vascular checks.
Imaging & Laboratory Tests
- Imaging
- X-rays: To assess for fractures, bone alignment, spurs, or arthritis
- MRI: Detailed images for soft tissues, ligaments, tendons (e.g., plantar fasciitis, ligament tears)
- Ultrasound: Helpful for tendon or ligament injuries, real-time soft tissue imaging
- CT scans: High-detail images for complex fractures or structural abnormalities
- Electrophysiological Tests
- Nerve conduction studies & electromyography (EMG): Evaluate nerve function, helpful in neuropathies or tarsal tunnel syndrome
- Laboratory Tests
- Blood tests: Rule out infections, inflammatory markers for arthritis, uric acid for gout
- Doppler studies: Assess blood flow in suspected vascular conditions
Treatments for Foot Pain
Treatment varies widely depending on the underlying diagnosis. Approaches include conservative management, medications, therapies, procedures, and surgery.
1. Conservative/Home Management
- Rest, Ice, Compression, Elevation (RICE): Standard for acute injuries and inflammation
- Activity modification: Avoid aggravating actions; temporarily reduce weight-bearing as needed
- Proper footwear & orthotics: Supportive shoes, custom arch supports, or inserts for flat feet or plantar fasciitis
2. Medications
- Over-the-counter pain relievers: Acetaminophen, NSAIDs like ibuprofen and naproxen for pain and inflammation
- Topical analgesics: Medicated creams or patches for localized relief
- Prescription medications: For severe pain or neuropathy (e.g., gabapentin, amitriptyline), COX-2 inhibitors, or corticosteroid injections for persistent inflammation
3. Physical & Support Therapies
- Physical therapy: Tailored exercises to stretch, strengthen, and rehabilitate the foot; gait retraining
- Night splints/braces: Hold foot in position overnight (commonly for plantar fasciitis)
- Massage and stretching: Improve circulation and reduce tension
4. Procedures & Surgery
- Minor procedures: Removal of corns, calluses, or ingrown toenails by a specialist
- Orthopedic surgery: Reserved for severe or non-responsive cases (complex fractures, severe bunions/hammertoes, chronic tendon rupture, or arthritis-induced deformity)
- Nerve blocks or ablation: For persistent nerve-related pain
5. Other Therapies
- Steroid injections: For severe inflammation not responding to other treatments
- Custom orthotic devices: To offload pressure and correct biomechanical problems
Prevention Tips
- Maintain a healthy weight to reduce pressure on the feet
- Wear properly fitted, supportive shoes; avoid prolonged use of high heels
- Stretch and strengthen foot and leg muscles regularly
- Promptly manage minor injuries to prevent worsening
- Control medical conditions that may affect the feet, such as diabetes, arthritis, and gout
- Seek medical advice for persistent, severe, or worsening foot pain
When to See a Doctor
Consult a healthcare provider if you experience:
- Severe or persistent pain, swelling, or visible deformities
- Signs of infection (redness, warmth, fever, discharge)
- Numbness, tingling, or burning (indicating possible nerve involvement)
- Inability to bear weight or walk
- No improvement with home care within a few days
Common Systemic Causes of Foot Pain
Your feet are particularly vulnerable to pain caused by arthritis, which can affect any of the foot's 33 joints. Arthritis-related foot pain often involves inflammation, stiffness, and swelling, making mobility challenging and sometimes leading to joint deformity or disability.
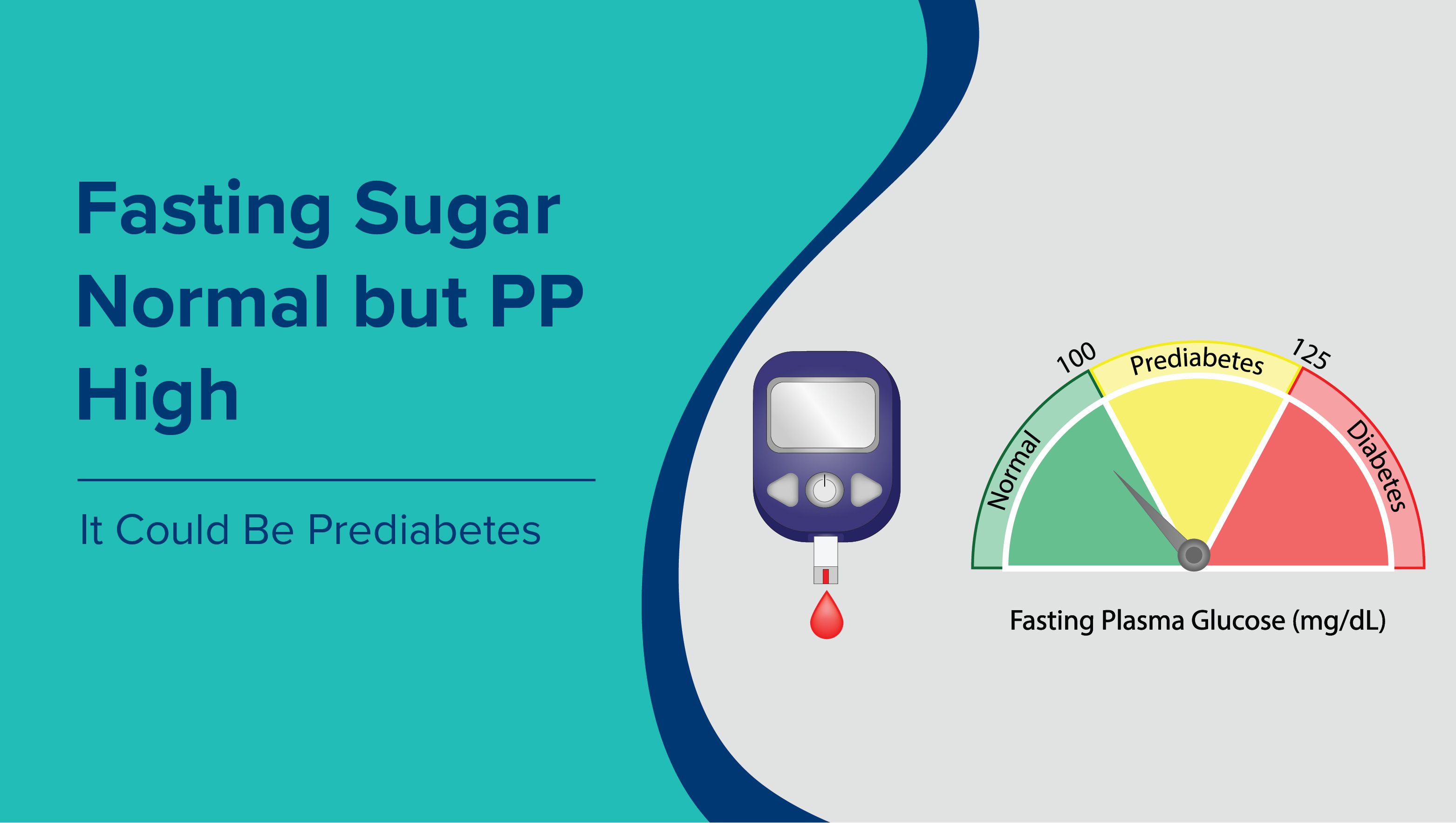
Diabetes mellitus is another major contributor to foot problems. People with diabetes are at higher risk for several foot disorders due to complications like:
- Nerve damage (diabetic neuropathy): Can cause numbness, tingling, burning, and loss of sensation in the feet, increasing the risk of unnoticed injuries or ulcers.
- Poor circulation (peripheral vascular disease): Reduces blood flow, impairing healing and making infections more likely.
- Foot ulcers or sores: Chronic wounds that can become infected and, in severe cases, may require amputation if not treated early.
Other important risk factors for foot pain include:
- Obesity: Extra body weight puts more strain on the feet, increasing wear and risk for joint and soft tissue issues.
- Pregnancy: Hormonal changes, additional weight, and altered gait can cause foot discomfort.
- Acute injuries: Conditions like sprains, fractures, or tendon injuries (such as tendinitis) may result in persistent pain if not properly treated.
Additional causes of foot pain encompass a wide range of conditions:
- Mechanical and anatomical issues: Corns, calluses, bunions, warts, ingrown toenails, and hammer toes develop due to friction, pressure, or abnormal bone alignment.
- Soft tissue and nerve conditions: Morton’s neuroma (thickening around a nerve), athlete’s foot (fungal infection), Haglund’s deformity (heel bone enlargement), and peripheral arterial disease can result in pain and function loss.
- Functional issues: Flat feet (fallen arches) and plantar fasciitis cause pain in the arch or heel, especially during walking or standing for prolonged periods.
- Systemic and inflammatory diseases: Gout and rheumatoid arthritis commonly affect the big toe and other foot joints, causing redness, swelling, and severe tenderness.
- Medication side effects: Some drugs may cause swelling and discomfort in the feet.
Ultimately, foot pain is a complex symptom with various potential causes. Arthritis and diabetes are leading contributors, but trauma, anatomical abnormalities, infections, and systemic diseases all play significant roles. Recognizing these factors and managing underlying health issues can help prevent or relieve foot pain and its complications
Summary
Foot pain can result from a variety of causes, each requiring a tailored approach for diagnosis and treatment. Early evaluation, appropriate diagnostic tests, and adherence to prescribed therapies can relieve symptoms, prevent long-term complications, and restore mobility and function. Always consult a specialist (such as a podiatrist) for accurate foot pain diagnosis and management suited to your unique needs.