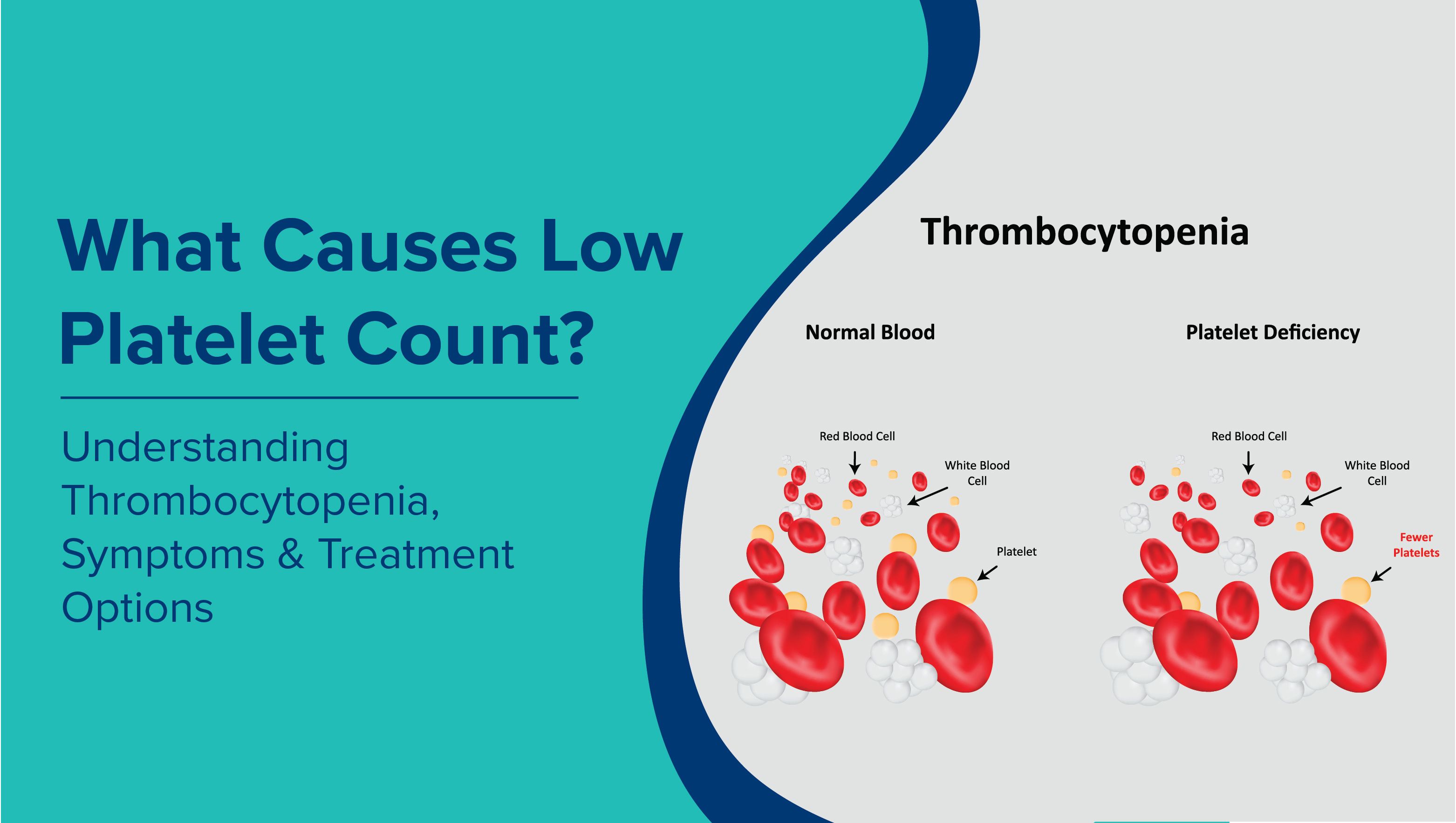
Platelets are small blood cells essential for blood clotting and preventing excessive bleeding. A low platelet count, also known as thrombocytopenia, can lead to bruising, prolonged bleeding, and in severe cases, life-threatening complications. Understanding the causes, symptoms, and treatment options is crucial for timely intervention.
What Is Thrombocytopenia?
Thrombocytopenia is a medical condition in which the blood has an abnormally low number of platelets, which help in clot formation to stop bleeding. A normal platelet count typically ranges from 150,000 to 450,000 platelets per microlitre of blood. When the count falls below this range, the risk of bleeding and bruising increases, which may require medical evaluation and management.
Types of Thrombocytopenia
Thrombocytopenia can be classified based on severity and duration:
Severity:
- Mild - Platelet count slightly below normal, often without major symptoms.
- Moderate - Lower platelet count that may cause easy bruising or prolonged bleeding from minor injuries.
- Severe - Very low platelet levels, increasing the risk of spontaneous bleeding, which can be life-threatening.
Duration:
-
Acute - Develops suddenly and usually resolves within weeks or months, often triggered by infections, medications, or other temporary factors.
-
Chronic - Persists for six months or longer and may be linked to ongoing conditions such as immune disorders, bone marrow problems, or chronic diseases.
What Level of Platelets Is Dangerous?
The clinical risk increases as platelet count decreases. While mildly low counts may not cause noticeable symptoms, progressively lower levels significantly raise the chances of bleeding and serious complications.
|
Platelet Count (per µL) |
Health Implication |
Usual Medical Approach |
|
150,000–450,000 |
Within normal range |
No specific action required |
|
100,000–150,000 |
Slightly below normal; often no symptoms |
Regular monitoring may be advised |
|
50,000–100,000 |
Increased risk if injured or during surgery |
Close observation, avoid unnecessary invasive procedures |
|
20,000–50,000 |
Spontaneous bleeding becomes possible |
Restrict use of blood-thinning drugs; medical review essential |
|
10,000–20,000 |
High chance of internal or mucosal bleeding |
Platelet transfusion may be recommended |
|
Below 10,000 |
Critical level; life-threatening bleeding, including brain |
Emergency transfusion and therapies like IVIG |
Platelet counts below 20,000 per µL are considered dangerously low, requiring immediate medical attention.
Normal Platelet Count Range: Male vs Female
A healthy platelet count is essential for blood clotting and preventing excessive bleeding. While the normal range is broadly the same, slight variations may be noted between men and women.
|
Gender |
Normal Platelet Count Range (per µL) |
Notes |
|
Male |
135,000 – 317,000 |
Standard adult range |
|
Female |
157,000 – 371,000 |
Slight fluctuations may occur during menstrual cycles or pregnancy |
Understanding these differences helps in assessing risks, especially in low platelet counts in pregnancy, where platelet levels may naturally decrease.
When to Seek Emergency Care
Low platelet counts can sometimes become life-threatening if bleeding occurs unexpectedly. It is important to recognise the warning signs that require urgent medical attention:
- Spontaneous or unexplained bleeding
- Frequent bruising
- Bleeding gums or nosebleeds
- Blood in urine or stool
- Unusual fatigue with bleeding signs
Prompt evaluation is essential when platelet levels are dangerously low.
Causes of Low Platelet Count
Thrombocytopenia, or low platelet count, can result from several underlying mechanisms. The major causes include:
- Decreased production of platelets due to bone marrow disorders
- Increased destruction by autoimmune diseases
- Sequestration of platelets in an enlarged spleen
A common cause of Low Platelet Count is Immune Thrombocytopenic Purpura (ITP).In this condition, the immune system mistakenly destroys platelets, reducing their numbers in the blood. ITP can affect both children and adults, and it often becomes chronic in adults. Common symptoms include easy bruising, small red spots on the skin known as petechiae, and prolonged bleeding from minor injuries. Treatment depends on the severity of the condition and may involve steroids, intravenous immunoglobulin (IVIG), or platelet transfusions.
Common Causes of Low Platelet Count in Adults and the Elderly
Thrombocytopenia may result from multiple factors:
Medical Conditions:
- Viral infections such as HIV, Hepatitis C, and Dengue fever (Dengue Ns1 Antigen Test)
- Cancer and chemotherapy
- Autoimmune diseases like lupus or rheumatoid arthritis
Medications:
- Heparin-induced thrombocytopenia
- Certain antibiotics and anticonvulsants
Lifestyle and Nutritional Factors:
- Excessive alcohol consumption
- Vitamin B12 or folate deficiency (Vitamin B12 testing may help)
Older adults may experience naturally lower platelet production due to age-related bone marrow changes.
Symptoms of Low Platelet Count
Low platelets can cause visible and internal symptoms, including:
- Easy or excessive bruising
- Petechiae, small red spots on the skin
- Prolonged bleeding from cuts or minor injuries
- Fatigue, weakness, or dizziness
Early recognition of these signs can prevent severe complications.
How Is Low Platelet Count Diagnosed?
Accurate diagnosis requires medical testing:
- Complete Blood Count (CBC): Measures platelet levels
- Bone marrow biopsy: Identifies underlying bone marrow disorders
- Antibody tests: Detect immune-related platelet destruction
Regular monitoring is important, especially in patients with known risk factors.
Treatment Options for Thrombocytopenia
Treatment depends on the underlying cause:
- Immune Thrombocytopenia: Steroids or IVIG
- Medication-induced low platelets: Discontinuation of causative drugs
- Severe thrombocytopenia: Platelet transfusions
- Underlying medical conditions: Addressing viral infections, autoimmune diseases, or nutritional deficiencies
Early intervention reduces the risk of complications and supports recovery.
Low Platelets in Pregnancy: What You Should Know
Mild drops in platelet count are common during pregnancy, a condition known as gestational thrombocytopenia, which usually develops in the third trimester. While this is generally harmless, severe or rapid declines in platelet levels may signal complications such as preeclampsia or HELLP syndrome. Regular monitoring is therefore essential to ensure both maternal and foetal safety.
Complications of Low Platelets
Low platelet count, or thrombocytopenia, is not just about bruising or prolonged bleeding. When levels drop dangerously, it can lead to severe and life-threatening complications.
Key complications include:
- Internal bleedingMay occur in organs such as the stomach or intestines, sometimes without obvious external signs.
- Brain haemorrhage A critical risk when platelet levels fall to dangerously low levels, requiring urgent medical care.
- Pregnancy-related risks Increased chances of heavy bleeding during delivery or complications linked to conditions like preeclampsia.
Tips to Maintain a Healthy Platelet Count
While not all cases of low platelets can be prevented, adopting healthy lifestyle habits can support better platelet production and function.
Practical tips include:
-
Eat a nutrient-rich diet Include foods high in Vitamin B12, folate, and iron, such as leafy greens, beans, citrus fruits, and lean meats.
-
Limit harmful substances Avoid excessive alcohol intake and processed foods that may impair bone marrow function.
-
Manage chronic conditions Conditions like diabetes, liver disease, or autoimmune disorders should be carefully monitored under medical guidance.
- Get regular health checks Periodic Complete Blood Count (CBC) tests help track platelet levels and detect changes early.
When to See a Doctor
Timely medical care is crucial when platelet levels drop. You should seek professional help if you experience:
- Persistent bruising or unexplained bleeding
- Platelet counts consistently below 50,000 per µL
- Sudden drops in platelet counts during pregnancy or after viral infections
Early evaluation and treatment reduce the risk of severe complications such as internal bleeding or organ damage. With convenient at-home diagnostic tests such as the CBC, Vitamin B12, and Dengue NS1 Antigen Test, MaxAtHome makes it simple to monitor platelet health without the need to visit a hospital. Professional sample collection and reliable reporting ensure timely care and peace of mind for you and your family. To book a test, reach out to us at 9240299624.
Frequently Asked Questions
What Does Low Platelet Count Mean?
A low platelet count, also called thrombocytopenia, occurs when the number of platelets in the blood falls below the normal range of 150,000 to 450,000 per microlitre. Platelets are essential for blood clotting, and a reduction in their number can lead to an increased risk of bleeding, bruising, and slower wound healing.
What Are the Symptoms of Low Platelet Count?
Low platelets may cause easy bruising, small red spots on the skin (petechiae), prolonged bleeding from cuts, nosebleeds, gum bleeding, and in severe cases, internal bleeding. Fatigue and weakness can also be present, reflecting the body’s response to blood loss.
What Causes Thrombocytopenia?
Thrombocytopenia can occur due to decreased platelet production, increased destruction, or abnormal sequestration in the spleen. Common triggers include bone marrow disorders, autoimmune diseases, certain medications, chronic illnesses, and nutritional deficiencies.
Can Stress Cause Low Platelet Count?
While stress alone rarely causes a significant drop in platelet levels, chronic physical or emotional stress may indirectly affect platelet production or worsen underlying conditions that lead to thrombocytopenia.
What Deficiency Causes Low Platelets?
Deficiencies in key nutrients such as Vitamin B12, folate, and iron can contribute to low platelet production. Ensuring adequate intake of these nutrients is essential for maintaining healthy platelet counts.
What Is the Fastest Way to Increase Platelets?
The approach depends on the underlying cause. For deficiency-related thrombocytopenia, correcting nutritional deficits with a diet rich in B12, folate, and iron is effective. In immune-mediated or severe cases, medical treatments such as steroids, IVIG, or platelet transfusions may be necessary under professional supervision.
When Does a Low Platelet Count Become Dangerous?
The clinical risk rises as platelet counts drop. Mildly low counts may not cause symptoms, but levels below 50,000 per microlitre significantly increase the risk of bleeding. Dangerously low counts, particularly under 20,000 per microlitre, can lead to severe bleeding, including internal haemorrhage, and require urgent medical attention.
Can Viral Infections Like Dengue Fever Cause Low Platelets?
Yes. Viral infections are a common cause of a drop in platelet count. Dengue fever, in particular, is well known for causing a sharp decline in platelets, which is why monitoring through tests such as the Dengue NS1 Antigen Test is important. Other viral infections, including HIV, Hepatitis C, and Epstein-Barr virus, can also contribute to low platelet levels. When platelet counts fall during infections, the risk of bleeding increases, making close medical observation and timely testing essential.
What Are the Effects of Low Platelets?
Low platelet levels increase the likelihood of bleeding complications, which can range from mild bruising to severe internal haemorrhage. It may also affect recovery from injuries or surgery and, in pregnant women, elevate the risk of complications during childbirth.
Can Diet Help Improve Platelet Count?
Yes. Nutrition plays a crucial role in supporting healthy platelet levels. Including foods rich in Vitamin B12 such as eggs, fish, and dairy, folate from spinach, legumes, and avocados, and iron from red meat, beans, and green leafy vegetables can help maintain or improve platelet counts. At the same time, it is advisable to avoid excessive alcohol and highly processed foods, as these can negatively affect platelet production. A balanced diet is especially important for recovery in cases where nutritional deficiencies contribute to low platelets.